First Person Stories: Getting an STI diagnosis
Reading Length: Mid read – 5 mins
This article touches on: STIs, sexual health
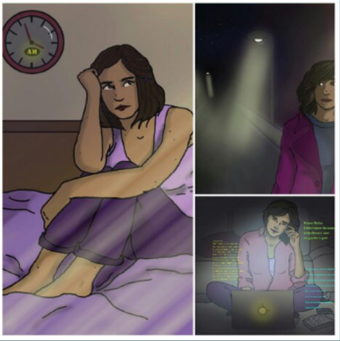
So, let’s start from the beginning… In 2016, I had just started University. Loving my new ‘adult’ life.
But was very quickly brought back to reality when I knew something wasn’t 100% right ‘down there’....
Like most overthinking teens, I rushed to google, searched in my symptoms and the first thing that came up was herpes.
My stomach dropped as I knew I couldn’t just ignore this… This wasn’t just going to magically disappear. I called up the local sexual health clinic, booked an appointment and anxiously waited. The nurse took one look and confirmed it was herpes.
This is the point where I should clarify what herpes actually is… Genital herpes is an STI passed on through vaginal, anal or oral sex. In the UK, about 70% will be infected with herpes by their 25th birthday. Most people who have herpes don’t develop symptoms, hence why it’s so easily transmitted. However, if you do show symptoms, it will usually flare up in the form of a small blister and can be treated with antibiotics, however it can come back. An important note about herpes, is that it’s part of the same family as cold sores and chickenpox, so it’s a viral infection. Like most viral infections, they can brought on by simply just being stressed or a lack of sleep.
I was sent on my way, with my antibiotics in hand, genuinely thinking my life was never going to be the same again. Can you tell I’m a drama queen yet??
From previous, negative experiences at college of people being outed for having STI’s, I kept my news private and only told a small circle of people. This resulted in me becoming fixated on the fact I couldn’t shake this part of my life away, which caused me to become extremely stressed and anxious, which (surprise) caused more herpes outbreaks. The problem with this is, it meant I couldn’t heal. By keeping it a secret, I was still creating shame that I had herpes, when in fact there’s nothing to be ashamed of.
It was only until I reached out to a mental health specialist, via my University, that I started to accept and process my new sexual identity. By openly talking about how my sexual health was coinciding with my mental health, I was able to pin-point certain triggers that were making my mental and sexual health outbreaks worse. Such as, attending uni in the day and working at night, caused me to constantly panic that I wasn’t resting enough and inevitably get more outbreaks.
Like any medical diagnosis, it can affect people completely differently, and it can be a learning process finding ways you can personally manage your symptoms. For myself, my herpes outbreaks were majority brought on by stress. So, by accepting that I had an STI, this was a huge factor in improving my overall health and moving forward.
4 years later and I can safely say those overwhelmingly anxious thoughts and triggers are past me. I became comfortable in the fact there is literally NOTHING to be ashamed of and I shouldn’t feel alone (remember 70% of the UK have herpes by the age of 25) …
I understand it can completely feel like this new diagnosis is going to be the bane of your life forever, but it doesn’t have to be. When I first got outbreaks, I would fall into a pattern of shaming myself for even getting it in the first place and feel isolated because I wouldn’t tell anyone why I was feeling so exhausted and poorly. Now, I’m able to confidently tell my partner and friends when I have an outbreak and give myself the self-care I need (usually a warm bath with Epsom salts and lots of rehydration).
I’m actually so open about it, me and my friend did a whole Instagram Live talking about it, which you can find here.
Where to go for more support
If you want to learn more about your sexual health visit our page all about – link “exploring Sexual Health”. Here we explain what to expect when getting an STI test and how to avoid STI’s with contraception.
Talking about sex can feel challenging at the best of times, let alone talking about STI’s. However, if you do find yourself at the clinic waiting for a diagnosis, you are NOT alone and there is support for you.
Here are some great, non-judgmental sites to have a look at, if you want to learn more about STI’s;
- Brook – A great charity offering both clinical sexual health services and education and wellbeing services for young people.
- SH24 – A NHS funded, 24 hour service offering sexual health advice and testing.
- Rise Above – A platform all about sharing our experiences, challenges and questions.
Sexual Health coincides with your mental health, so it is completely normal to feel like your mental health is being affected by your sexual health (and vice versa).
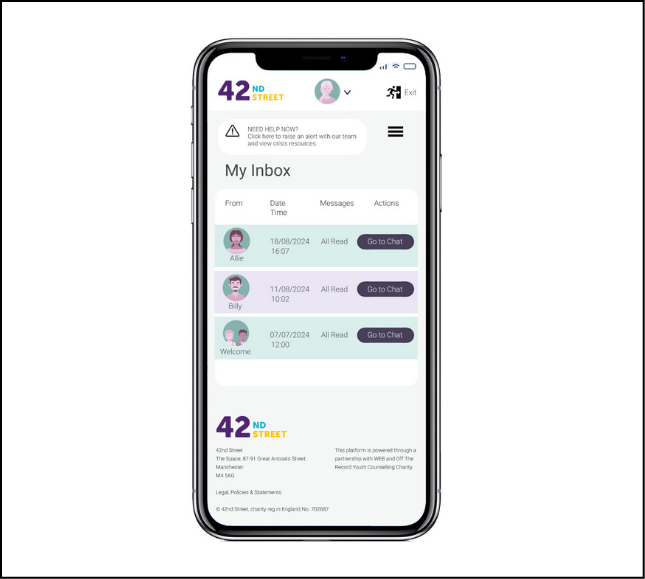
If you feel this is the case, you can chat to someone online via text, you can register for ongoing online support via our online support portal. We also hold weekly drop-in sessions so that you can speak with a worker without an appointment.
We provide a number of face-to-face services too, all of which offer something slightly different depending on what’s best for you. Overall, though, every service provides you with someone who will listen, acknowledge your feelings, and work with you to explore where your panic attacks might come from. You can read about our services here.
By: Daisy Wakefield